American
![]() f
Manual
Medicine
f
Manual
Medicine
|
American
|
Home
Search
Pain referral
Trigger points
Cranial nerve
Spinal nerve
Historical
About us
Contact us
Site map
Distinguishing features of these conditions are as follows: While both syndromes can be observed in both genders and all age groups, fibromyalgia has a higher preponderance of onset with females over 40. Trigger point pain only discriminates between genders with preponderance and referral pattern pertaining to individual muscle syndromes; examples for preponderance toward females are TMD, pectoralis major and pelvic floor. Fibromyalgia has a softer, more subtle clinical representation of musculature with range of motion relatively unaffected even though a cardinal indicator is morning joint stiffness. Conversely, myofascial disorders exhibit taut muscle bands or buttony masses that when snapped transversely will elicit a pain referral. Due to the shortened or hypertonic state of these muscles, a decreased range of motion should be manifest. While pain associated with fibromyalgia can be quite intense, it usually is of a more diffuse nature and is seldom described as a deep aching or sharp shooting knife-like referral.
While there is a strength deficit with myofascial pain disorders, fatigue is indicative of fibromyalgia. However, this may be due to another cardinal indicator of non-restorative sleep. This non-restorative sleep pattern and fatigue must be differentiated from other symptoms associated with chronic fatigue syndrome, lupus erythematous, thyroid conditions and other systemic diseases such as coronary artery disease and metastatic cancer.
The tender point exam consists of the practitioner applying approximately 8 pounds of pressure with pincher type palpation to 9-paired anatomical sites, yielding 18 points of contact. Upon sudden non-sustained application of pressure to any one of these 18 sites, should the individual wince, grimace, or withdraw from the practitioner, the site is considered positive. Eleven or more positive responses are indicative of further diagnostic work-up. In addition to the conditions referenced above, mixed connective tissue disease can also elicit a positive tender point finding. Examples of mixed connective tissue disease to be differentiated are polymyalgia rheumatica, temporal arteritis and polymyositis.
Locations of tender points for exam: click on a small image to view an enlarged image
Home
Search
Pain referral
Trigger points
Cranial nerve
Spinal nerve
Historical
About us
Contact us
Site map
Continuing Education © Copyright
Tender Point Exam For Generalized
Or Migrating Myalgia
The tender point exam is most frequently used in determining fibromyalgia. However, it should be noted that as a stand-alone physical exam it proves only point tenderness with positive findings being presumptive of generalized or migrating myalgia, with etiology unknown. For
fibromyalgia, a positive finding consists of 11 out of 18 points registering hypersensitivity, as well as other cardinal indicators or factors being present. Prior to establishing this condition as being fibromyalgia, numerous other conditions must be eliminated through blood work, electro- and/or radiographic findings, as they also can elicit similar results. Lupus erythematous, polymyositis, dermatomyositis, polymyalgia rheumatica, thyroid conditions, and cancer may also yield these same concomitants. Numerous authors consider fibromyalgia and myofascial pain syndrome to be essentially one in the same condition. Dr.’s Travell and Simons noted marked distinctions between the two. These authors’ professional experience seems to support Travell and Simon’s delineation. While there may be trigger points located within tender points, not all tender points are trigger points. Acute myofascial pain is sudden in onset, and usually only involves one well-defined quadrant without migration. Fibromyalgia is insidious, migratory and must be present for over 6 months in duration. It is accompanied with morning joint stiffness and non-restorative sleep, as well as a wide array of other symptomatology. Chronic myofascial pain in more than one region is somewhat more difficult to qualify from fibromyalgia, especially in view of the fact that it is possible for both syndromes to coexist.
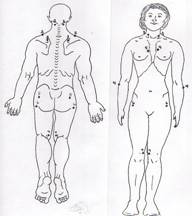
The American Arthritis Association recommends the following points of contact for the Tender point exam: